Treatment
The treatment options for Castleman disease are specific to the subtype diagnosed by your physician.
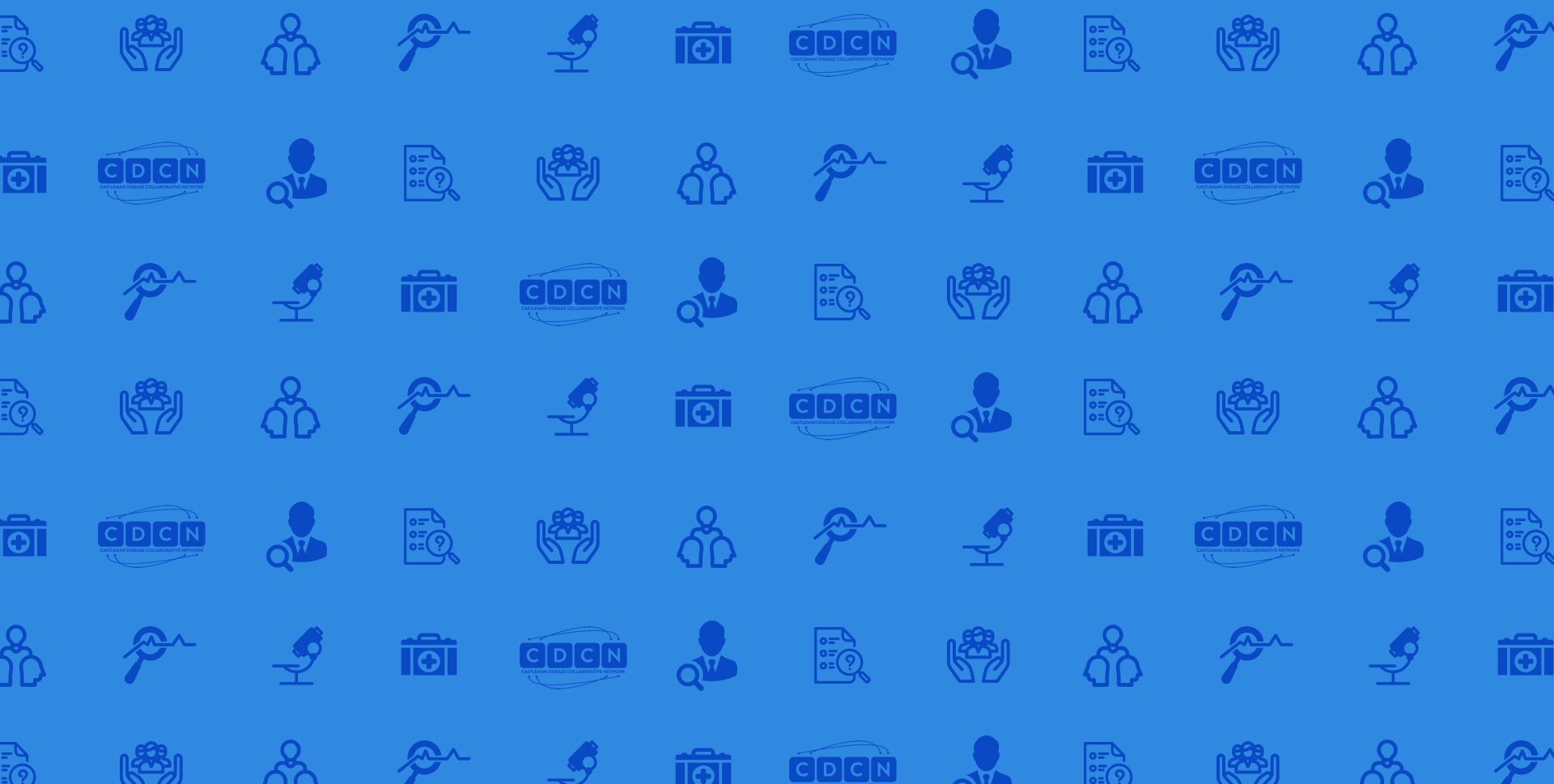
Unicentric Castleman disease (UCD): Surgery is considered by experts to be the first-line treatment for almost all cases of UCD. A patient is considered cured of UCD if their enlarged lymph node or nodes are removed completely and any previous clinical/laboratory abnormalities return to normal. Sometimes, removing the enlarged lymph node(s) is not possible. If surgical excision is not possible, treatment is recommended for symptomatic patients. If symptoms are due to compression, then rituximab may be administered to attempt to shrink the enlarged lymph node. Some UCD patients may experience inflammatory symptoms (fever, fatigue) and elevated inflammatory laboratory markers after lymph node excision. These patients are sometimes treated with treatments frequently used to treat MCD, such as anti-IL-6 therapy with siltuximab. If these treatments are not effective, then radiation is sometimes tried.
People with unicentric Castleman disease usually do well once the affected lymph node is removed and life expectancy is usually not changed. However, people with unicentric Castleman disease are at increased risk of developing paraneoplastic pemphigus (PNP), which is a rare autoimmune condition that can be deadly. Paraneoplastic pemphigus involves blisters in the mouth and on the skin that are often misdiagnosed. Though the risk of developing paraneoplastic pemphigus is still low (<5%) among people with unicentric Castleman disease, it is the most deadly potential complication and should be evaluated in all UCD patients at the time of diagnosis and following diagnosis to ensure that treatment is rapidly initiated if it presents.
There are no reported cases of UCD transforming into MCD. Your medical team will discuss the options and risk for surgery depending on the location of the enlarged lymph nodes. More information on the current treatment guidelines can be found here:
*UCD patients should be evaluated for lymph node resectability, with surgery being the preferred method of treatment. Consider presurgical embolization in large vascular UCD lymph nodes to render surgery safer. Follow-up CT scans, physical examination, and laboratory testing can be done at 12-month intervals. In rare patients who continue to have symptoms after complete lymph node excision, other diagnoses and/or treatments should be considered.
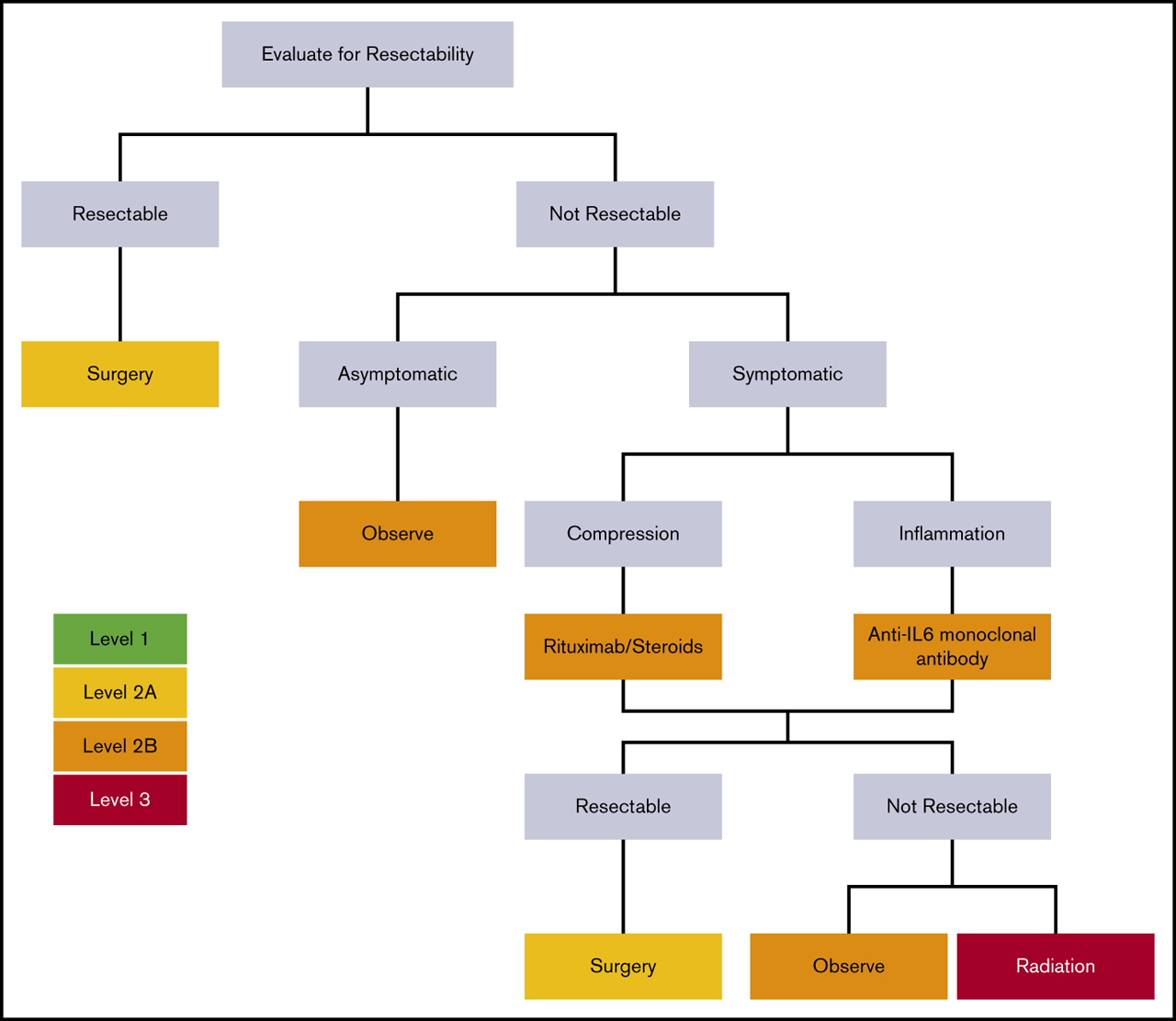
HHV-8 associated multicentric Castleman disease (HHV-8+MCD): Rituximab is recommended as first-line therapy for HHV-8+ MCD. It is highly effective, but occasionally antivirals and/or cytotoxic chemotherapies are needed. Rituximab targets and eliminates B cells, a special type of immune cell. This is an advantage of rituximab, as traditional chemotherapy drugs eliminate many types of cells and therefore result in different side effects. The degree of immunosuppression is also milder than traditional chemotherapy drugs. Your medical team will discuss the side effects you can expect from rituximab. Further information can be found here.
HHV-8 negative/idiopathic Multicentric Castleman disease (iMCD): First-line treatment for idiopathic multicentric Castleman disease is anti-IL-6 therapy with siltuximab (or tocilizumab, if siltuximab is not available). Siltuximab (Sylvant) is the only FDA-approved treatment for iMCD and patients who responded to siltuximab tend to have long-term responses. This drug targets a specific protein (interleukin-6) that is highly involved in inflammation. Unlike traditional chemotherapy, anti-IL6 therapy is more targeted and doesn’t result in the elimination of any cell types so the side effects are milder. The amount of immunosuppression will be dependent on whether other drugs are used simultaneously. Anti-IL-6 therapy is effective in about 34-50% of patients, but some patients do not respond o it. In these cases, rituximab, autoimmune disease treatments, or chemotherapy regimens used for blood cancers are used. In critically ill patients, corticosteroids are recommended and adjuvant chemotherapy is needed if the patient is demonstrating disease progression while on siltuximab. Corticosteroids such as prednisone can help control inflammation and chemotherapies can eliminate rapidly proliferating immune cells. In patients where siltuximab is not effective, other treatments such as rituximab and sirolimus (Rapamune) can be used. Unfortunately, rituximab tends to not work as successfully in iMCD patients compared to HHV-8 associated MCD patients.
In patients who have both multicentric Castleman disease and POEMS syndrome (POEMS-associated MCD), treatment should be directed at the POEMS syndrome.
More information on the current treatment guidelines for MCD can be found here:
To learn more about management of iMCD, read the most recent publication here.
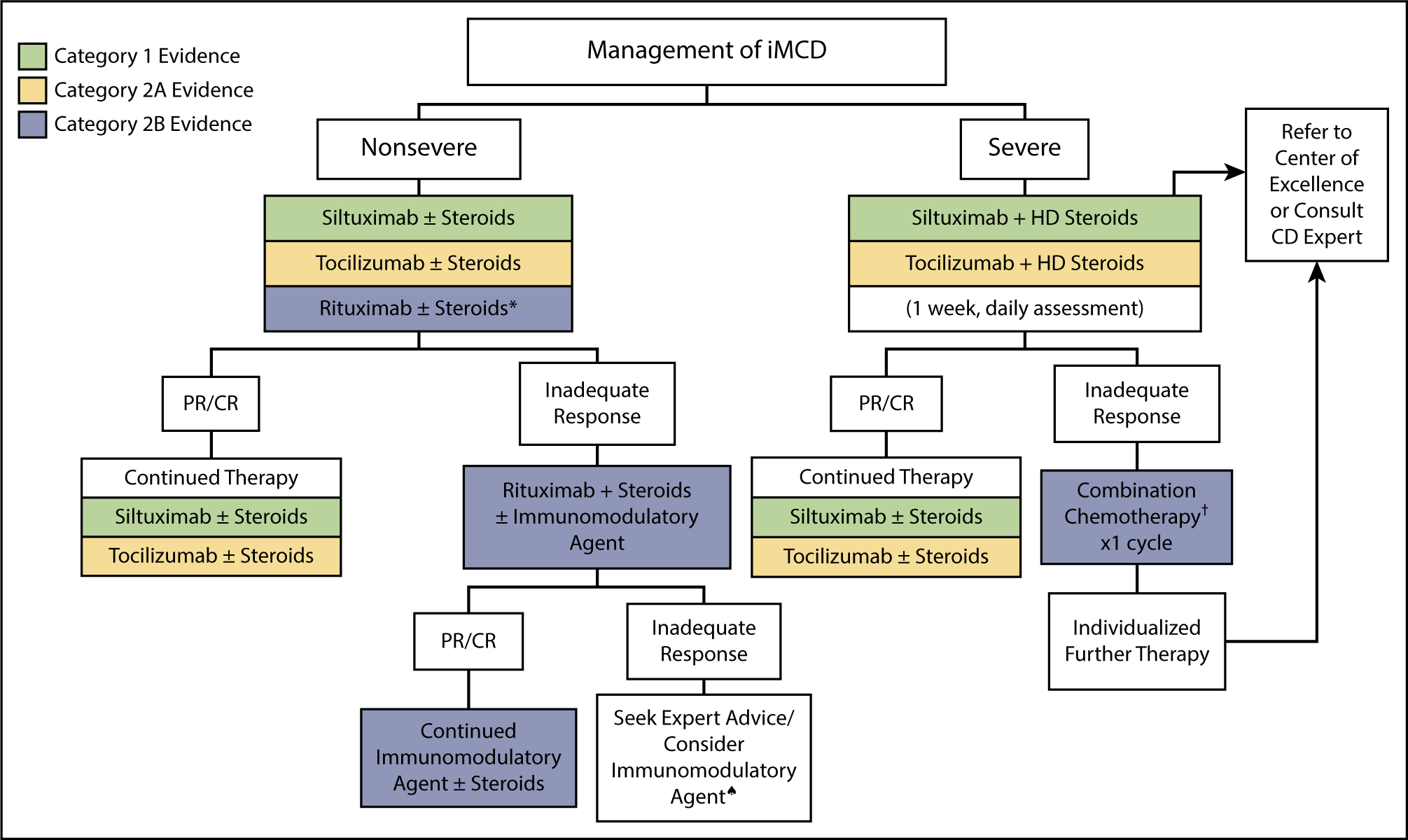
The above Figure is taken from the CDCN’s recommended treatment guidelines for iMCD and is also generally consistent with the National Comprehensive Cancer Network guidelines for treatment of iMCD (B cell lymphomas, Version 3 2021).
**The side effects of treatment will be very specific to the treatment chosen by the medical team.
The good news is that in the last decade, an explosion in Castleman disease research has identified new targets and there is hope new treatments will emerge soon.
A clinical trial for the medication sirolimus for iMCD patients who did not improve on siltuximab or tocilizumab was recently conducted. Patients can learn more about this trial at cdcn.org/sirolimus. The trial has been posted to the federal registry for all clinical trials here.
For more information about treatment options for MCD, you can visit hemonc.org/wiki/Castleman_disease.