From Medical Student to Patient: 26 Days in a Hospital
“I would like to start you on cyclophosphamide and etoposide this afternoon,” my oncologist said to me as I was lying in my hospital bed, now two weeks into my stay. I never anticipated I would be on the receiving end of some of the harshest chemotherapy drugs I would help administer as a future physician, yet there I was about to receive them. I couldn’t stop my mind from instantly leaping towards thoughts of losing my hair, incessant vomiting, and urinating blood, side effects of these drugs I had learned about while studying for my first board exam literally weeks earlier. And now here I was about to receive them. 
About three weeks prior, I was walking back home after picking up my lab results from my school clinic. Gradually over the past month, I had started becoming more tired and short of breath to the point that I was regularly falling asleep while studying and getting winded after walking up a single flight of stairs. Looking down at my lab results, I was baffled. ‘Low hemoglobin, low platelets, elevated creatinine’ were just a few of the abnormal results. I knew what some of them meant individually, but together, I couldn’t make sense of them. Over the next few days, I noticed other odd symptoms. My ankles had swollen and, after casually stepping on a scale, realized I had gained 14 lbs over the previous few weeks. My school clinic doctor had recommended repeating my initial labs in a few more days given the aberrancies, but by this point, my friends and family were telling me to go to the ER so that’s what I did.
At the ER check-in desk, when asked about my reason for coming, I told them, “hyperkalemia, pitting edema, and 14 lb. weight gain”. I then sat down, proud that I had finally put some fancy medical jargon to good use. Within 20 or so minutes my name was called and I was brought to a patient room. After a few hours of questioning and lab draws in the ER, I was told I would be admitted because it looked like my kidneys weren’t functioning properly.
Over the next couple of days, not much changed. I must have explained my “story” at least a dozen times to physicians across multiple specialties, including hematology-oncology, nephrology, and infectious diseases. My doctors also printed and provided me my daily labs at my request. The only thing I could piece together from the results with my fledgling two years of medical school experience was that they kept getting worse. I remember one physician confessing that he didn’t quite know what was going on with me but then went on to utter an adage well-known to those in medicine, “When you hear hoofbeats, think horses not zebras”, alluding to the teaching that doctors should focus on the likeliest possibilities when making a diagnosis, not the unusual ones. I would, at a later time, smirk from the irony of his choice of words.
One afternoon after getting the results of my pan-CT scan, one of the residents sat at the edge of my bed. With a somber expression on her face she told me that nearly all of my lymph nodes were enlarged. “Lymphoma?”, I asked, curious to finally get some answers. She said maybe, but they wouldn’t know for sure until they did bone marrow and lymph node biopsies. After she left, I immediately opened up my computer and started Google searching the prognosis of lymphoma. Did I have Stage 3? Stage 4? Hodgkin’s? Non-Hodgkin’s? Is a 90% survival-rate at 5 years supposed to be good? Rather than get emotional, it seemed I had opted for intellectualization as my psychological defense mechanism.
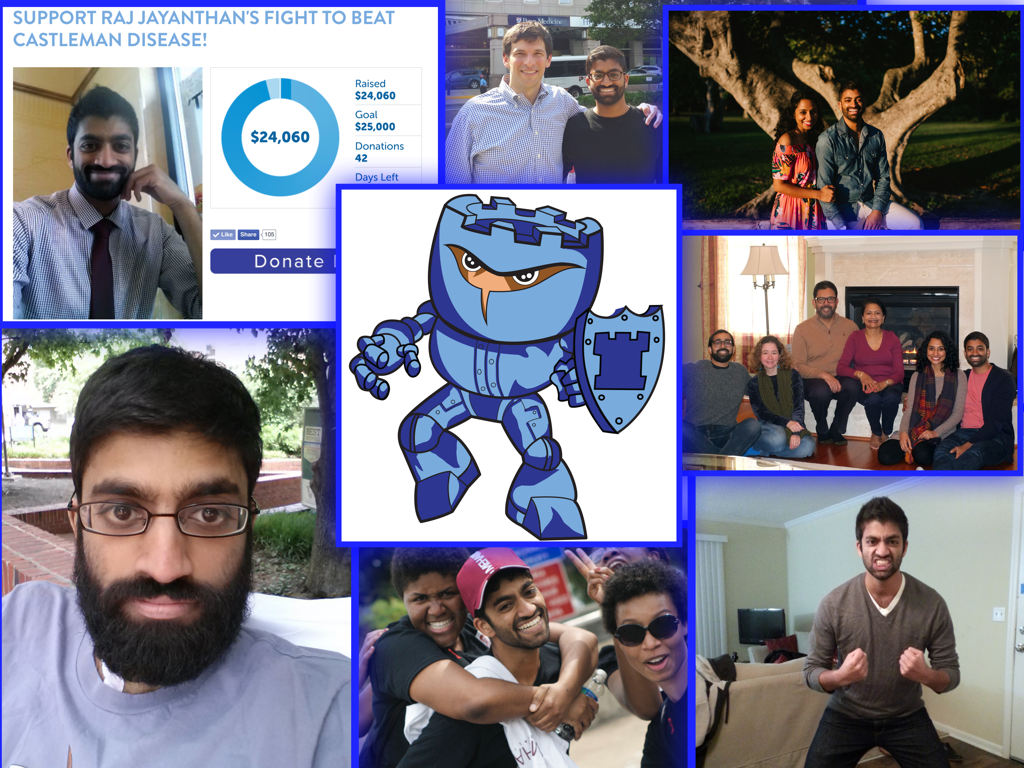
 One week after being admitted, my oncologist walked into my room and told me she finally had a diagnosis for me. “Have you heard of Castleman disease?” she asked. Having never learned about it in my two years of medical school, I said no. She explained that my kidneys and bone marrow were failing and this disease was the cause. She added that it was rare, poorly-understood, usually found in the elderly, and that I had the multicentric variant, an even less common type of Castleman disease with more widespread effects. She also stated it was idiopathic, which I knew meant doctor’s had no idea what caused it. On my initial Google searches of the disease, I found a brief and unhelpful Wikipedia page and the website of a Castleman disease organization that looked like it hadn’t been updated in 10 years. I didn’t know what to make of everything. Should I be happy it wasn’t cancer? Or worried that my oncologist believed I may be the fourth case of idiopathic multicentric Castleman disease based on her review of the literature? Though I would later learn this was untrue, I continued to remain emotionally stoic about it all and probably too physically weak to really comprehend what was going on with me until sometime after I left the hospital.
One week after being admitted, my oncologist walked into my room and told me she finally had a diagnosis for me. “Have you heard of Castleman disease?” she asked. Having never learned about it in my two years of medical school, I said no. She explained that my kidneys and bone marrow were failing and this disease was the cause. She added that it was rare, poorly-understood, usually found in the elderly, and that I had the multicentric variant, an even less common type of Castleman disease with more widespread effects. She also stated it was idiopathic, which I knew meant doctor’s had no idea what caused it. On my initial Google searches of the disease, I found a brief and unhelpful Wikipedia page and the website of a Castleman disease organization that looked like it hadn’t been updated in 10 years. I didn’t know what to make of everything. Should I be happy it wasn’t cancer? Or worried that my oncologist believed I may be the fourth case of idiopathic multicentric Castleman disease based on her review of the literature? Though I would later learn this was untrue, I continued to remain emotionally stoic about it all and probably too physically weak to really comprehend what was going on with me until sometime after I left the hospital.
Despite having a diagnosis going into my second week of hospitalization, my doctors’ treatments weren’t working and I was only getting worse. All the muscle and fat in my body were atrophying. About a month ago before getting sick, I weighed 150 lbs. Now, I was 193 lbs. Despite the muscle and fat loss, I was retaining a substantial amount of fluid in my legs and abdomen. So much so that I needed a wheelchair to get around and a parent or nurse’s help to get dressed every day. With the amount of fluid I was retaining and kidneys that had deteriorated to the point of virtually no urine output, I was told I would need to begin dialysis.
Three weeks in, it felt as if my doctors had thrown the whole kitchen sink at me and weren’t getting anywhere. Rituximab, chemo, steroids, broad antibiotics–none of it seemed to be helping. Even the four-hour sessions of dialysis every other day weren’t enough to prevent fluid from accumulating in my lungs, which ultimately required an incredibly painful procedure to drain. The disease and medication side effects were taking its toll. I remember glimpsing at the mirror at one point and seeing for the first time what cachexia looked like. I was so physically weak I couldn’t even feel ashamed about accidentally vomiting all over myself or my episodes of incontinence.
While all this was going on, my parents, who had flown in to stay with me soon after I was hospitalized, were wasting no time looking for outside help. While the hospital I was at was well-known and reputable, it was easy for my parents to see that my doctors weren’t entirely comfortable with what they were treating. My parents reached out to any physician friends and family members they knew who in turn conferred with their own network of physician colleagues. Eventually, contact was made with a Castleman disease physician-scientist at the NIH, who promptly began consulting with my hospital’s doctors about my case. Late into my third week, I was given what I would later realize was my life-saving drug, tocilizumab. Within days my kidneys began to improve, my depleted cell counts started to rise, and I was feeling better. So much so that just six days after that single dose of tocilizumab, I was discharged.
I spent the following weeks back home recovering with regular lab visits and twice-a-month tocilizumab infusions. With my kidneys soon returning to nearly 100% function, I was urinating out 2-3 lbs worth of water-weight daily. Two months after leaving the hospital, I returned back to medical school to restart studying for my board exam.
Today, I’m proud to have been off treatment and in remission for nearly six years. I’m also humbled by my fortune, as many patients with multicentric Castleman disease lose their battle to it, and those that survive require regular maintenance therapy to do so. My experience has afforded me a unique perspective on medicine from the eyes of a patient and I’m not sure I could have acquired it any other way. I hope these memories will remain with me long into my years as a physician in order to influence my medical decisions for the betterment of my patients.